Abstract
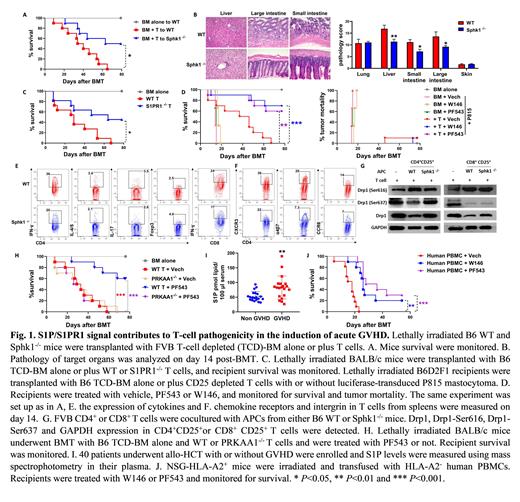
Allogeneic hematopoietic cell transplantation (allo-HCT) is a curative option for the treatment of hematological malignancies, which is primarily mediated by donor immune cells. Acute graft-versus-host disease (aGVHD) mainly induced by transplanted donor T cells is a major and life-threating complication leading to severe "cytokines storm" and multiple organ damage, which contributes to high morbidity and mortality and thus limits the success of allo-HCT. Sphingosine-1-phosphate (S1P), a bioactive lysophospholipid, is synthesized from sphingosine by sphingosine kinase 1 (Sphk1) or Sphk2 and degraded by S1P lyase. S1P signal plays an important role in regulating biological functions and homeostasis of T lymphocytes, and thus has been considered as a therapeutic candidate against autoimmune disease. In current study, we demonstrated that Sphk1 but not Sphk2 is required for antigen-presenting cells (APC) to activate allogeneic T cells. Using murine allo-HCT models, we found that secretory S1P produced by Sphk1 in the recipients was required for the development of full-blown GVHD (Fig. 1 A-B). Consistently, S1PR1, a primary receptor for S1P, plays a critical role in the pathogenicity of donor T cells to induce GVHD (Fig. 1C). Using pharmacologic inhibitors, we demonstrated that specific inhibition of Sphk1 (PF543) or S1PR1 (W146) substantially attenuated GVHD while preserving graft-vs.-leukemia (GVL) effect (Fig. 1D). Mechanistically, S1P/S1PR1 signal facilitated T-cell activation and differentiation towards Th1/Th17 but away from Tregs (Fig. 1E) and also promoted T-cell migratory potential into GVHD target organs (Fig. 1F). S1P/S1PR1 signaling increased mitochondrial fission of pathogenic CD4 + T cells through PRKAA1 dependent Drp1 and phosphorylated S6 (pS6) activation (Fig. 1 G-H). Whereas CD8 + T cells were much less sensitive to S1P-S1PR1-PRKAA1-pS6/Drp1 axis, which likely contributed to the GVL maintenance when S1P/S1PR1 signaling is absent or inhibited (Fig. 1 D, G). Furthermore, clinical data demonstrated that patients with acute GVHD exhibited a comparable level of sphingosine but a significantly higher level of S1P, as compared to the patients without GVHD, suggesting a positive role of S1P in GVHD development in clinic (Fig. 1I). Finally, we validated the efficacy of inhibiting Sphk1/S1PR1 in GVHD prevention induced by human T cells in a xenograft model (Fig. 1J). Taken together, our results provide a rationale and novel mechanism of targeting Sphk1/S1PR1 in the prevention of GVHD and leukemia relapse after allo-HCT. This novel strategy may be translated in the clinic to benefit patients with hematologic malignancies.
No relevant conflicts of interest to declare.